Institute Presentation
Leiden University is an internationally oriented, comprehensive University. Our scientific research and teaching inspire one another, and this cross-pollination shapes our contribution to society. With our research, we work to gain a fundamental understanding of the world and the people around us. In our teaching, we train our students to become analytical thinkers and critical world citizens who can apply this knowledge to make the world a safe, healthy, sustainable, prosperous and just place. Where possible, we endorse and apply the Sustainable Development Goals of the United Nations.
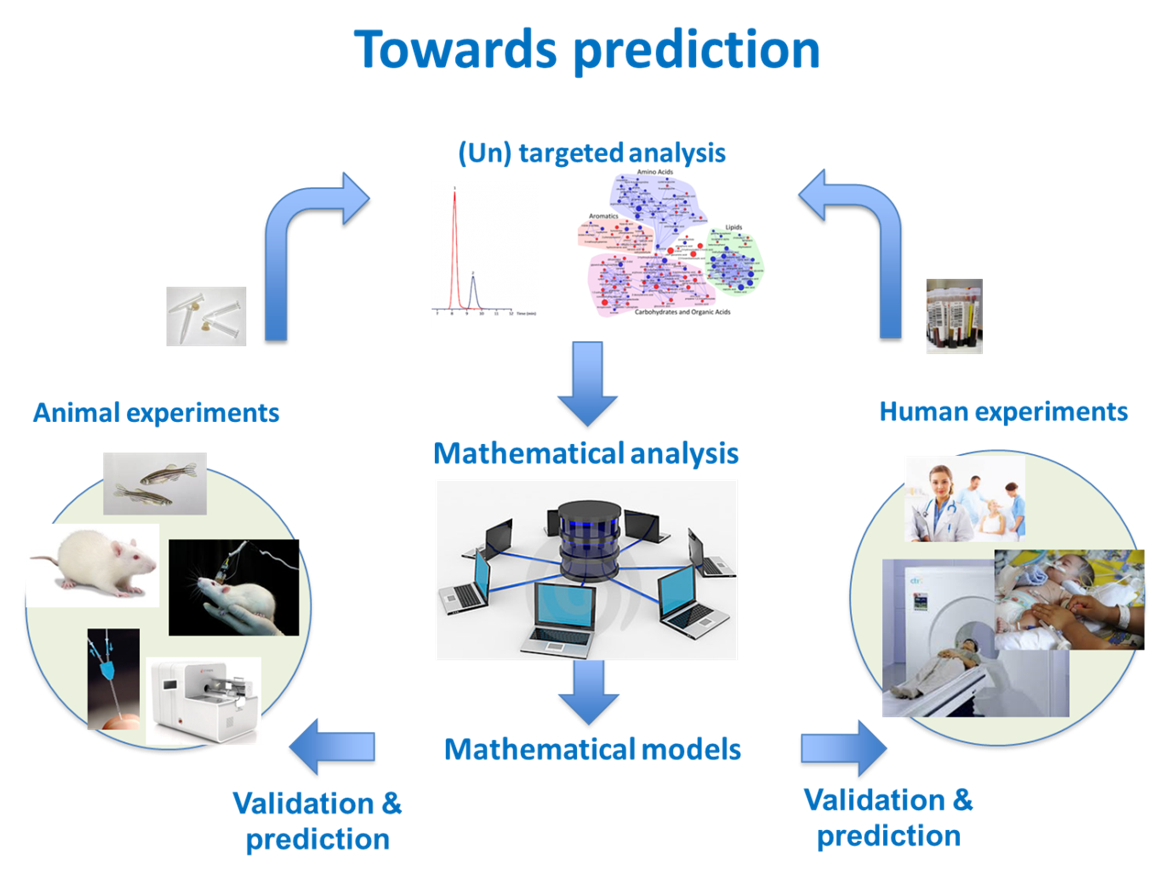
The Leiden Academic Centre of Drug Research (LACDR) is one of the Institutes of the Faculty of Science, and our Division of Systems Biomedicine and Pharmacology is one of the three divisions there. In this division, our aim lies in the development of personalised medicine strategies, and development of new systems-based approaches in translational and clinical pharmacology. To that end, we aim for a thorough understanding of diseases, at the system-level, and is aimed at predicting the modulation of disease networks by drugs in cells, organs, and the body as a whole. To achieve this, we gather pharmacokinetic, metabolomic and pharmacodynamic data from preclinical in vitro and in vivo models, as well as from patients or patient-derived material (i.e. organ-on-a-chip models using human iPSC derived cells), which we integrate into systems pharmacology modelling. In this division, Prof. Dr. Elizabeth de Lange is leading the Predictive Pharmacology research group, where research is based on the ‘Mastermind Research Approach’.
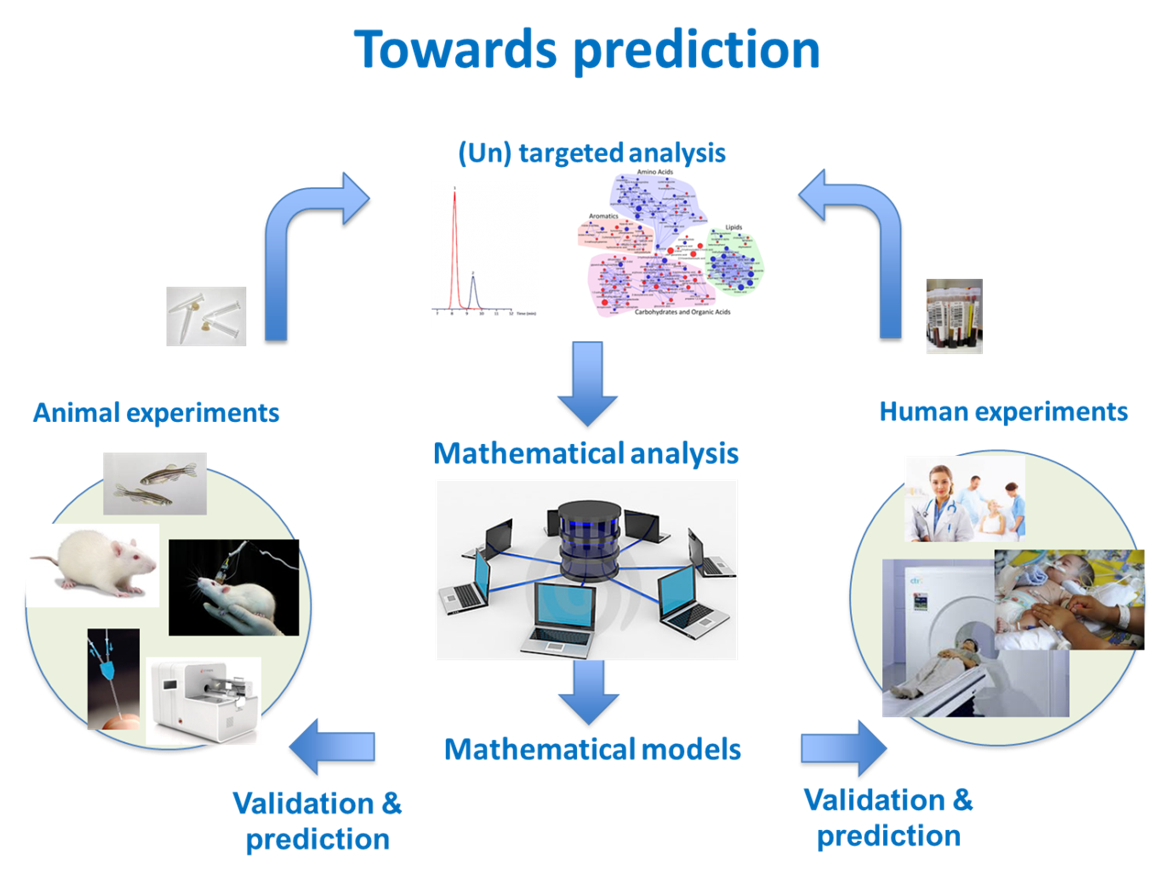
Figure caption: In the Predictive Pharmacology research group, strategic experimental studies, designed to have smart data, and modelling studies go hand-in-hand. The ultimate goal is to predict pharmacokinetics and pharmacodynamics of medicines in human, under health and diseased conditions, with already a number of successes.
Prof. Dr. Elizabeth de Lange was the scientific leader and coordinator of the QSPainRelief consortium as well as work package leader of WP3 on data collection (from literature, existing external databases, and newly generated QSPainRelief data), data storage (database), and data reuse for development of the QSPainRelief Model Platform for predicting best medicine combinations of treating chronic pain in individual patients. Towards this end, the use and further development of ULEI’s CNS PBPK model to predict CNS target site concentrations of medicines (in WP2, together with ISB) was instrumental.